In-situ simulation (ISS) is a form of simulation-based learning that takes place in real clinical settings, with benefits including the identification of system vulnerabilities, refinement of protocols and improvement of inter-professional dynamics, all without endangering patients [1]. This theoretical basis for learning is underpinned by situativity theory and principles such as the systems engineering initiative for patient safety (SIEPS) [2]. We report on the use of ISS prior to the relocation and expansion of two existing ICUs totalling 31 beds into one new purpose-built 55-bed facility, as part of a redevelopment of the Royal Sussex County Hospital in Brighton.
A number of high-fidelity multidisciplinary simulations were held in the new facility prior to relocation, followed by detailed documented team debriefs to identify safety themes. Simulations included unanticipated cardiac arrest and difficult intubation. Scenarios were conducted in a variety of open bays and negative pressure side rooms to maximise learning. Additional timed simulations were conducted for time-critical ITU transfers such as the computed-tomography (CT) scanner, theatre complexes and interventional radiology suites.
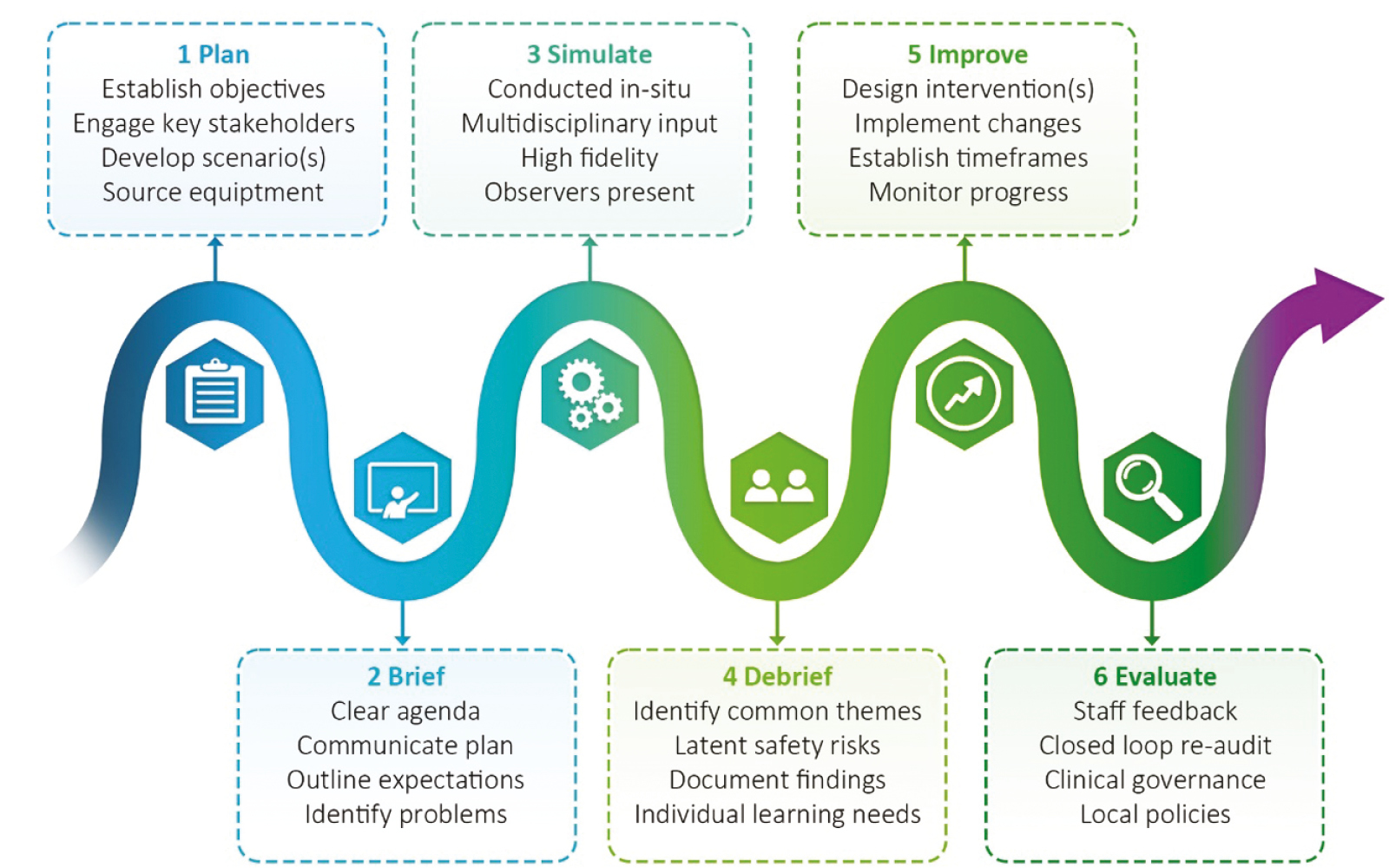
Key themes were the accessibility of emergency equipment as well as challenges in the ergonomics and layout of the new unit. Barriers to emergency medication access and the need for improvements to the bedspace nomenclature were also raised. Feedback from staff was universally positive with common themes being a greater level of preparedness and familiarity with the new environment. The simulations also identified potential challenges with staffing templates on the new unit. As illustrated in Figure 1-A6, safety issues were fed back to their relevant medical and nursing leads to develop strategies to improve safety.
We highlight the successful implementation of ISS within a QI framework to aid the safe relocation and expansion of a large critical care facility. We are now exploring the ongoing use of multidisciplinary ISS on the new critical care unit, with other scenarios such as raised intracranial pressure under development. Critical aspects of this model are the need for key stakeholder buy-in and staff engagement at all levels, with appropriate senior oversight throughout.
Authors confirm that all relevant ethical standards for research conduct and dissemination have been met. The submitting author confirms that relevant ethical approval was granted, if applicable.
1. Calhoun AW, Cook DA, Genova G, Motamedi SM, Waseem M, Carey R, et al. Educational and patient care impacts of in situ simulation in healthcare. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare. 2024;19(1S).
2. Carayon P, Schoofs Hundt A, Karsh B-T, Gurses AP, Alvarado CJ, Smith M, et al. Work system design for patient safety: The SEIPS model. Quality in Health Care. 2006;15(suppl 1):i50–8.