
Interprofessional simulation-based education (IPSE) is a relatively new pedagogical strategy in health professions education curricula in Africa. Therefore, there is a paucity of literature on the implementation of IPSE and the current practice of IPSE in Africa. This scoping review seeks to identify, synthesize and map the evidence base for IPSE at the undergraduate level in health professional institutions in Africa.
This scoping review will explore the literature on IPSE in undergraduate health profession programmes. It will consider any IPSE activity in Africa, across diverse settings, including designated simulation classrooms, clinical and community settings on any healthcare topic, or clinical skill.
The Joanna Briggs Institute guideline for Scoping Reviews will be used to identify and appraise the relevant literature. The databases to be searched include PubMed, CINAHL, PROSPERO, SCOPUS, the Open Science Framework, Cochrane Database of Systematic Reviews, Embase and ERIC. The search will include publications and gray literature. Reference lists of eligible studies will be back-searched. The findings will be summarised in tabular form and a narrative synthesis will inform recommendations and areas for future research and practice.
After completion of their tertiary education, healthcare professionals are expected to work as a team with other healthcare colleagues, utilizing their skills to collaboratively deliver high-quality, safe patient care [1]. However, because of the structure of undergraduate healthcare education globally, healthcare students are typically not exposed to working or learning collaboratively [2,3]. It is suggested that this siloed pedagogical approach is a ‘root cause of sentinel events in hospitals’ [4] (p.241). In contrast, the literature suggests that interprofessional education (IPE) can produce a collaboration-ready workforce [2,4,5]. IPE occurs ‘when students from two or more professions learn about, from and with each other to enable effective collaboration and improve health outcomes’ [6] (p.7).
There is a heightened appreciation of IPE in healthcare education institutions worldwide [1,5–7]. Organizations, such as the Centre for the Advancement of Interprofessional Education (CAIPE) [8] and the Interprofessional Education Collaborative (IPEC) [5], have been instrumental in providing guidelines on and advocating for the implementation of IPE globally [5]. The IPEC framework for interprofessional collaborative practice was first published in 2011, revised in 2016 and again in 2023. This framework outlines the core competencies healthcare professionals should achieve during their education [9] and is organized into four domains: values and ethics, roles and responsibilities, communication, and teams and teamwork [5]. This framework for interprofessional practice has helped to create commonality in IPE programmes worldwide, enabling measurement and comparison of outcomes [9].
Similarly, CAIPE, advocates for active, interactive, reflective and learner-centred teaching methods in IPE, including case-based learning, and simulated learning [8]. However, research findings indicate that simulation is the preferred approach for delivering IPE [1,10,11]; these studies indicate that interprofessional simulation-based education (IPSE) gives students an experience where they can rehearse real-world clinical scenarios, exchange professional information and challenge established hierarchies. While simulation is recognized as a means of fostering interprofessional collaborative practice among healthcare students, there are geographical disparities in IPSE research globally. Most of the published evidence comes from Western, Educated, Industrial, Rich and Democratic (WEIRD) countries. Conversely, there is limited evidence on IPSE in Africa, and the extant literature has not been aggregated to explore and understand the contextual factors surrounding the implementation of IPSE. Therefore, it is imperative to address this gap in understanding, given the unique challenges and healthcare landscape in Africa.
Africa is characterized by diverse cultures and varied healthcare systems [3]. Many African countries face health challenges, such as poor quality maternal and child health, and high incidences of non-communicable and infectious diseases [3,12]. These challenges are exacerbated by limited healthcare resources, which necessitate a coordinated and cooperative approach to healthcare [3,12]. However, health professional education in Africa does not prepare students to work in a collaborative environment [3,12]. This has resulted in professional tribalism [3], with different professions acting independently of one another or even in competition, potentiating a detrimental effect on patient outcomes [3,12]. A lack of contemporary research on the implementation of IPSE in Africa raises concerns about the preparedness of healthcare professionals to address the complex and evolving healthcare needs of diverse African populations [3]. The current practice of IPSE in Africa needs to be better understood, and this scoping review aims to illuminate the contextual factors peculiar to the African milieu, adding to the continuing global discourse on IPSE.
The conceptual framework for this scoping review will be guided by the IPEC core competencies for interprofessional collaborative practice: Version 3 (5) (see Figure 1).

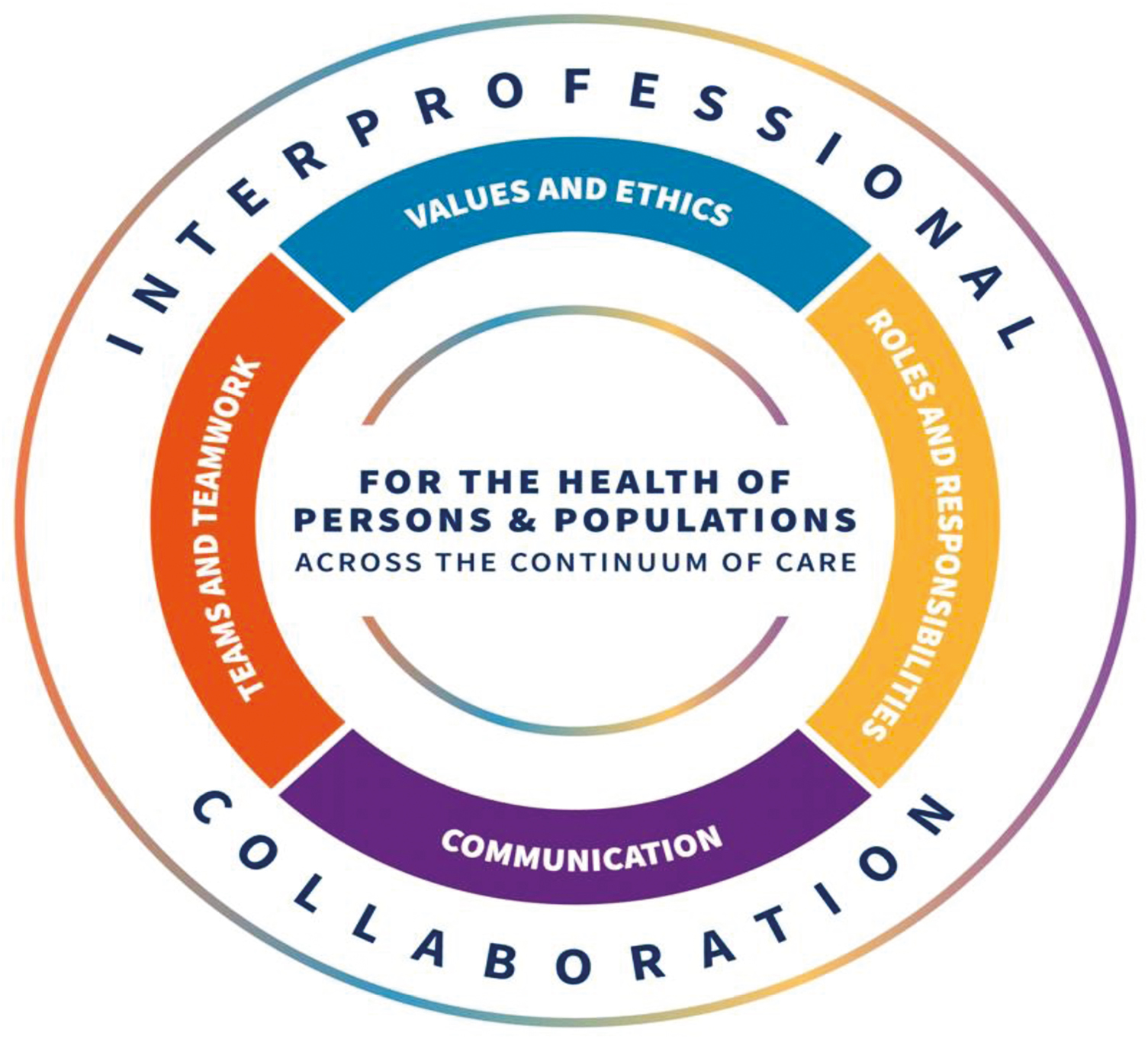
IPEC Core Competencies for Interprofessional Collaborative Practice: Version 3 (5) (p.15).
The IPEC core competency framework was developed to guide the development, implementation and assessment of IPE activities [13], and it provides a conceptual lens for analysing IPSE programmes in Africa for this scoping review. In addition to facilitating an understanding of how well the programmes align with globally recognized standards, the IPEC framework will also help to identify gaps and strengths in the current IPSE initiatives in Africa. The IPEC framework’s emphasis on core competencies will focus the review on essential aspects of interprofessional practices that are critical in healthcare outcomes. Adopting this conceptual approach will ensure the credibility and rigour of this scoping review, making the findings applicable for future IPSE implementation in Africa.
This scoping review seeks to identify, synthesize and map the evidence base for IPSE at undergraduate level in healthcare education institutions in Africa.
1.What is the scope of IPSE activities in Africa?
2.What are the characteristics of undergraduate IPSE activities in the African context?
3.What are the factors that constrain or support the implementation of undergraduate IPSE activities in Africa?
This review will utilize the Participant, Context and Concept mnemonic as recommended by the Joanna Briggs Institute (JBI) guideline for scoping reviews [14] to determine the study inclusion criteria.
The review will focus on undergraduate IPE activities involving simulation conducted in Africa. The included studies will involve simulations with at least two different healthcare professional student groups.
This review will encompass studies that describe the implementation, outcomes, challenges and best practices of IPSE.
The review will consider any IPSE activity in Africa, which involves experiential learning activities, across diverse settings, including designated simulation classrooms, and clinical and community settings on any healthcare topic or clinical skill.
Studies will be excluded if they do not describe IPSE activities in Africa; involve only one professional group and do not involve simulation. Articles published before 2004 and in languages other than English will be excluded.
This review will be conducted according to the JBI scoping review guidelines [14]. Therefore, in line with this approach, the following steps will be followed:
1.Search strategy
2.Study selection
3.Data extraction
4.Data analysis and presentation
The review will be reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses extension for Scoping Reviews (PRISMA-ScR) framework as recommended by Tricco et al. [15].
A search strategy will be developed in consultation with a research librarian with the goal of identifying published studies from peer-reviewed journals as well as gray literature. Using Medical Subject Headings (MESH), index terms, search terms or phrases, synonyms and alternative terms, a search of the published literature will be carried out. The following search terms and phrases, along with their respective synonyms will be used: interprofessional education, simulation-based education, healthcare students, and healthcare professionals. The Boolean operators ‘OR’ and ‘AND’ will be combined to produce search strings (see Appendix I).
The database search will encompass PubMed, CINAHL, PROSPERO, SCOPUS, CINAHL, the Open Science Framework, Cochrane Database of Systematic Reviews, Embase, ERIC, ProQuest Dissertation, Google Scholar and JBI Register for Scoping Reviews. In addition to scholarly databases, the search will encompass gray literature from relevant organizations including the Africa Interprofessional Education Network, World Health Organization, CAIPE and IPEC. The reference lists of included papers will also be searched to locate any additional references relevant to the review.
Following the database search, identified records will be collated and uploaded into Endnote20 and duplicates will be removed. The search results will then be uploaded into Rayyan for title and abstract screening. A two-stage standardized screening process will be employed to evaluate the eligibility of identified records. Therefore, three reviewers (GN, SS and NH) will independently screen the title and abstracts of the captured records. Any disagreements during this process will be mediated through discussions with BK. Full-text articles of the included studies will then be downloaded for in-depth review. Full-text papers that do not match the inclusion criteria will have their exclusion reasons documented and reported in the scoping review. The search findings will be fully documented in the scoping review and displayed in a form that adheres to PRISMA-ScR.
The data extraction process will involve a two-phased approach to ensure accuracy and rigour. In the first phase, a modified JBI data extraction tool (see Appendix II) will be piloted on a subset of the included studies to test its usability and effectiveness. Reviewers’ feedback from this pilot exercise will be used to refine and update the tool as necessary. All modifications to the data extraction tool will be transparently reported in the scoping review, to ensure clarity and reproducibility of the methodology.
In the second phase, we will use the updated tool to log the relevant articles. GN and SS will independently extract data from all included studies. NH will then verify the extracted data to ensure consistency and trustworthiness. Any disagreement or uncertainty in the extracted data will be resolved through discussion among the three reviewers, with BK acting as an adjudicator if consensus cannot be reached. Regular meetings will be held among the authors to facilitate this process.
The findings relevant to the review questions will be summarised in tables, figures and a narrative summary, depending on which presentation style is most suitable. Descriptive statistics will be utilized to summarise quantitative data, while content analysis will be utilized to synthesize qualitative data analysis [16].
Since this is a scoping review, no ethical approval is required. The findings will be disseminated through presentations at both national and international fora and published in a peer-reviewed journal. This scoping review is part of a multiphase study; therefore, the findings will guide the subsequent phases of the study and will contribute towards a Doctor of Philosophy in Medical Education.
We sincerely thank Mr. Scott McGregor the academic Librarian at the University of Dundee, for his expert assistance in developing the initial search strategy for this scoping review protocol. His valuable contributions provided a strong foundation for our research, ensuring a thorough and systematic approach to identifying relevant literature.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
Not applicable.
No potential conflict of interest was reported by any of the authors.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.

| 1 | ((((((((((((((((((((students, medical[MeSH Terms]) OR (students, nursing[MeSH Terms])) OR (students, dental[MeSH Terms])) OR (education, nursing[MeSH Terms])) OR (education, medical[MeSH Terms])) OR (medical students[Title/Abstract])) OR (nursing students[Title/Abstract])) OR (healthcare students[Title/Abstract])) OR (midwifery students[Title/Abstract])) OR (dental students[Title/Abstract])) OR (anesthetist students[Title/Abstract])) OR (radiology students[Title/Abstract])) OR (physiotherapy students[Title/Abstract])) OR (optometry students[Title/Abstract])) OR (learn*[Title/Abstract])) OR (curriculum[Title/Abstract])) OR (education*[Title/Abstract])) OR (teach*[Title/Abstract])) OR (train*[Title/Abstract])) OR (student*[Title/Abstract])) OR (skill*[Title/Abstract]) | 2,157,212 |
| 2 | ((((interprofessional[Title/Abstract]) OR (collaboration[Title/Abstract])) OR (exchange[Title/Abstract])) OR (interprofessional relations[MeSH Terms])) OR (interprofessional education[MeSH Terms]) | 464,123 |
| 3 | ((((simulation training[MeSH Terms]) OR (patient simulation[MeSH Terms])) OR (computer simulation[MeSH Terms])) OR (simulated[Title/Abstract])) OR (simulation[Title/Abstract]) | 660,187 |
| 4 | (Africa[Title/Abstract] OR Africa*[Title/Abstract] OR Algeria[Title/Abstract] OR Angola[Title/Abstract] OR Benin[Title/Abstract] OR Botswana[Title/Abstract] OR “Burkina Faso”[Title/Abstract] OR Burundi[Title/Abstract] OR Cameroon[Title/Abstract] OR “Canary Islands”[Title/Abstract] OR “Cape Verde”[Title/Abstract] OR “Central African Republic”[Title/Abstract] OR Chad[Title/Abstract] OR Comoros[Title/Abstract] OR Congo[Title/Abstract] OR “Democratic Republic of Congo”[Title/Abstract] OR Djibouti[Title/Abstract] OR Egypt[Title/Abstract] OR “Equatorial Guinea”[Title/Abstract] OR Eritrea[Title/Abstract] OR Ethiopia[Title/Abstract] OR Gabon[Title/Abstract] OR Gambia[Title/Abstract] OR Ghana[Title/Abstract] OR Guinea[Title/Abstract] OR “Guinea Bissau”[Title/Abstract] OR “Ivory Coast”[Title/Abstract] OR “Cote d’Ivoire”[Title/Abstract] OR Jamahiriya[Title/Abstract] OR Kenya[Title/Abstract] OR Lesotho[Title/Abstract] OR Liberia[Title/Abstract] OR Libya[Title/Abstract] OR Libia[Title/Abstract] OR Madagascar[Title/Abstract] OR Malawi[Title/Abstract] OR Mali[Title/Abstract] OR Mauritania[Title/Abstract] OR Mauritius[Title/Abstract] OR Morocco[Title/Abstract] OR Mozambique[Title/Abstract] OR Mozambique[Title/Abstract] OR Mocambique[Title/Abstract] OR Namibia[Title/Abstract] OR Niger[Title/Abstract] OR Nigeria[Title/Abstract] OR Principe[Title/Abstract] OR Reunion[Title/Abstract] OR Rwanda[Title/Abstract] OR “Sao Tome”[Title/Abstract] OR Senegal[Title/Abstract] OR Seychelles[Title/Abstract] OR “Sierra Leone”[Title/Abstract] OR Somalia[Title/Abstract] OR “South Africa”[Title/Abstract] OR “St Helena”[Title/Abstract] OR Sudan[Title/Abstract] OR Swaziland[Title/Abstract] OR Tanzania[Title/Abstract] OR Togo[Title/Abstract] OR Tunisia[Title/Abstract] OR Uganda[Title/Abstract] OR “Western Sahara”[Title/Abstract] OR Zaire[Title/Abstract] OR Zambia[Title/Abstract] OR Zimbabwe[Title/Abstract] OR “Central Africa”[Title/Abstract] OR “Central African”[Title/Abstract] OR “West Africa”[Title/Abstract] OR “West African”[Title/Abstract] OR “Western Africa”[Title/Abstract] OR “Western African”[Title/Abstract] OR “East Africa”[Title/Abstract] OR “East African”[Title/Abstract] OR “Eastern Africa”[Title/Abstract] OR “Eastern African”[Title/Abstract] OR “North Africa”[Title/Abstract] OR “North African”[Title/Abstract] OR “Northern Africa”[Title/Abstract] OR “Northern African”[Title/Abstract] OR “South African”[Title/Abstract] OR “Southern Africa”[Title/Abstract] OR “Southern African”[Title/Abstract] OR “sub Saharan Africa”[Title/Abstract] OR “sub Saharan African”[Title/Abstract] OR “sub-Saharan African”[Title/Abstract]) OR (Africa, South of the Sahara[MeSH Terms]) | 691,457 |
| 5 | 1 and 2 and 3 and 4 | 56 |
IPSE DATA EXTRACTION INSTRUMENT
Exclusion by title and abstract
Articles will be excluded by title and or abstract based on the following criteria.
1.Any article that is not health related
2.Any article which is health related, but is not about interprofessional education (IPE)
3.Any article which is not written in the English language
Data Extraction Instrument

| Author(s): |
| Publication Year: |
| Title of the Study: |
| Journal/Source: |
| Country(ies) of Focus: |
| Study Design: |
| 1. Which health professional students are involved in Interprofessional Simulation Education (IPSE)? (include numbers): select all that apply. A. Medical students B. Nursing students C. Pharmacy students D. physiotherapy student E. Dentistry (Dental Students) F. Social Work (Social Work Students) G. Public Health (Public Health Students) H. Speech-Language Pathology students I. Medical Laboratory Science J. Nutrition/Dietetics (Nutrition/Dietetics Students) K. Midwifery (Midwifery Students) L. Chiropractic (Chiropractic Students) |
| 2. Which faculty members are involved in IPSE? A. Medical B. Nursing C. Pharmacy D. physiotherapy E. Dentistry F. Social Work G. Public Health H. Speech-Language Pathology (Speech-Language Pathology) I. Medical Laboratory Science J. Nutrition/Dietetics K. Midwifery L. Chiropractic |
| 3. What types of interprofessional simulation-based activities are used at your institution? (Select all that apply): a. Virtual IPE b. Standardized patient c. Case-based discussions d. Simulated clinical rounds |
| 4. What equipment and resources are commonly used in the simulation activities at your institution? (Select all that apply): a. High-fidelity simulators (e.g. mannequins) b. Virtual simulation software c. Standardized patients (actors) d. Basic medical equipment (e.g. stethoscopes, IV bags) e. Classroom and laboratory space f. Other (please specify) |
| 5. Main healthcare topics covered in the IPSE activity. Select all that apply. A. Cardiovascular conditions B. Respiratory conditions C. Musculoskeletal conditions D. Gastrointestinal conditions E. Reproductive conditions F. Nervous conditions G. Endocrine conditions H. Renal and urinary conditions I. Integumentary conditions J. Immune and lymphatic conditions K. Reproductive and genitourinary conditions L. Public and community health M. Emergency medical services (EMS) N. Telehealth and health information |
| 6. Which IPE competencies are targeted in the IPSE activities? a. Teamwork and collaboration b. Communication skills c. Roles and responsibilities d. Conflict resolution e. Ethics and professionalism f. Patient-centred care g. Cultural competence h. Other (please specify) |
| 7. Where did the IPSE activity take place? A. Classroom B. Skills lab C. Clinical sites D. In situ |
| 8. Fidelity levels of IPSE as reported. A. High fidelity B. Low fidelity |
| 9. What are the reported enablers of IPSE? a. Strong institutional support and funding b. Availability of trained faculty and staff c. Access to high-quality simulation equipment and resources d. Positive attitudes and buy-in from students and faculty e. Effective integration into the curriculum f. Collaborative partnerships with healthcare organizations g. Other (please specify) |
| 10. What are the reported barriers to implementing IPSE? a. Limited funding and resources b. Insufficient training for faculty and staff c. Resistance to change from students or faculty d. Lack of time in the curriculum e. Inadequate access to simulation equipment f. Logistical challenges (e.g. scheduling, space) g. Other (please specify) |
| 11. What cultural considerations are considered in the design of your simulation activities? a. Inclusion of culturally relevant scenarios b. Sensitivity to language and communication styles c. Respect for traditional healthcare practices d. Adaptation to local healthcare contexts and practices e. Involvement of community members in simulation design f. Addressing cultural attitudes towards interprofessional collaboration g. Other (please specify) |
| 12. How is feedback from participants used to improve the IPSE programme at your institution? a. Regular review and revision of simulation scenarios b. Incorporation of participant suggestions into programme design c. Continuous professional development for faculty based on feedback d. Implementation of formal feedback mechanisms (e.g. surveys, focus groups) e. Sharing feedback with all stakeholders for collaborative improvement f. Adjustment of teaching methods and materials g. Other (please specify) |
| 13. How frequently are simulation-based IPE activities conducted at your institution? a. Weekly b. Monthly c. Quarterly d. Annually e. Never |
| 14. What equipment and resources are commonly used in the simulation activities at your institution? a. High-fidelity simulators (e.g. mannequins) b. Virtual simulation software c. Standardized patients (actors) d. Basic medical equipment (e.g. stethoscopes, IV bags) e. Classroom and laboratory space f. Other (please specify) |
| 15. What measurement instruments or approaches are used to evaluate the effectiveness of simulation-based IPE activities? a. Pre- and post-tests b. Observational checklists c. Student self-assessment surveys d. Peer assessments e. Faculty evaluations f. Standardized assessment tools (e.g. OSCE) g. Other (please specify) |
| 16. What contextual factors or presage conditions are reported in interprofessional simulation-based education in Africa? a. Availability of trained faculty b. Institutional support and funding c. Access to simulation technology d. Curriculum integration e. Student engagement and participation f. Cultural attitudes towards IPE g. Other (please specify) |
| 17. How have universities driven the expansion of IPE? a. Establishment of dedicated IPE programmes or centres b. Integration of IPE into existing curricula c. Faculty development and training programmes d. Collaboration with healthcare facilities for clinical placements e. Hosting workshops and conferences on IPE f. Policy advocacy and funding initiatives g. Other (please specify) |
| 18. What are the preferred ways of delivering IPE in the African context? a. Simulation-based activities b. Interprofessional clinical placements c. Collaborative classroom-based learning d. Online and virtual learning modules e. Community-based projects f. Interprofessional workshops and seminars g. Other (please specify) |
| 19. What is the reported impact of IPSE on health outcomes in Africa? a. Improved patient safety and quality of care b. Enhanced teamwork and communication among healthcare professionals c. Increased student confidence and competence d. Better understanding of professional roles and responsibilities e. Positive feedback from patients and community members f. No significant impact reported g. Other (please specify) |
| 20. Is the IPSE activity integrated in the curriculum? A. Yes B. No |
| 21. At what stage of the students’ training period is IPSE conducted at your institution? a. Early stage (first or second year) b. Mid stage (third or fourth year) c. Late stage (final year) d. Throughout the entire training period e. During clinical placements or internships f. Other (please specify) |
| 22. If reported what IPSE competency framework is followed? A. IPEC B. ASPIRE C. TeamSTEPPS D. CAIPE |