
Healthcare simulation and debriefing practices are optimal tools in health professions education and rely on a well-built psychologically safe construct for effectiveness and success. However, it is not well understood how differences working in solo or group scenarios impact learner preferences on learning outcomes and maintenance of psychological safety. This study aimed to uncover the sentiment of learners towards comfort with engaging in healthcare simulation through factors that confer psychological safety. These sentiments were examined in relation to satisfaction with achievement of learning objectives. The ability to leverage solo or group participants as an intentional design feature has implications for creators of simulation curricula. With intentionality, the determination of participant number for simulation-based education may prove to enhance individualized growth while supporting a psychologically safe environment that carries through to the debriefing phase.
This was a cross-sectional, observational study involving nurses and medical residents. Surveys were conducted using demographics, Likert-style questions and free-text responses. One hundred seventy-one learners participated. The primary outcome was perceived level of comfort by the participant. Secondary outcomes were participant preference, perceived psychological safety, self-confidence, conduciveness to learning, anxiety and realism to actual patient care.
One hundred seventy-one participants were enrolled. Respondents who experienced both solo and group learner scenarios were compared to those who experienced group scenarios only. Those who experienced both scenarios reported a strong association with overall level of comfort, satisfaction with scenario outcome, ability to make educated guesses and take risks (gamma > 0.3). Increased comfort with both scenario structures was strongly associated with an increasing number of simulation experiences.
Participants of healthcare simulation endorsed high levels of comfort and favourable components of psychological safety when past experiences included a combination of both modalities. Curriculum development with a purposeful design decision to incorporate both modalities may maximize learner outcome, target debriefing considerations and demonstrate the psychological safety link existing within the educational design.
What this study adds:
•This study examines how participants’ feelings about solo and group scenarios relate to their perceived learning outcomes.
•Understanding participants’ comfort levels in both solo and group scenarios could help inform scenario and debrief design.
•Results suggest that considering structural factors (such as solo vs. group scenarios) that contribute to psychological safety early in scenario development process may enhance perceived learning outcomes.
•This study lays the groundwork for further research into how participant comfort in simulation scenarios relates to outcomes of learning assessments and translation to bedside care.
Simulation-based activities have emerged as one of the optimal environments for healthcare education. Learners participate in scenarios involving patient care using manikins without risk or harm to actual patients. The ability to participate meaningfully is heavily rooted in the ability of the learners to feel psychologically safe to do so. Afterwards, a debriefing session provides time for an expression of learner emotion and reflection on the activity through guided facilitation [1–3]. It is this reflection upon action that provides the critical step of elucidating reasons behind one’s choices or decisions, which is referred to as a frame [4]. Understanding and adjusting one’s frames are crucial components of experiential learning and to do so also requires a psychologically safe learning environment that fosters learner engagement. The concept of psychological safety emphasizes that learners are free to take risks or make educated guesses without fear of punishment or ridicule and is an essential cornerstone of advancing one’s ability to make connections translatable to bedside care [2,3]. Experiential learning is relational at its core, and therefore preferences of learners, including the size of their simulation participant group, may hold a crucial link to enhancing psychological safety during simulation. Knowledge of these preferences may allow for purposeful incorporation of psychologically safe features from scenario design through to the debriefing phase. Examination of participant perception on size of the learning group and how those perceptions are associated with features of psychological safety has not yet been explored.
Simulation centres have differing ways in which they teach their learners; an important but perhaps not always deliberate choice is consideration of whether to implement a single-participant or a multiple-participant simulation format. Looking at learner perceptions on choice of format can provide insight into how participants learn and recall educational experiences. Furthermore, entering into a scenario with additional learners immediately changes the dynamic of the experience, which should be considered when constructing learning outcomes. Much work goes into the design of a simulation-based learning activity, yet despite careful objective writing and planning, the success of the learning outcome leans on the ability of the participants to fully engage in what was designed. The implications of psychological safety are present throughout all aspects of healthcare simulation and, as described by Purdy et al., hold a bidirectional impact that reaches to and is influenced by the healthcare environment itself [5]. Psychological safety begins much earlier than the start of the scenario, as it inherently exists even in the choices of the scenario designers, including the seemingly impactful decision of whether to build a solo or a group learner format.
Previous research in neurology, surgery and obstetrics examined personal preference and experience in a single-learner or multiple-learner scenario format. In these contexts, comfort was examined with procedural-based or technical skill as opposed to the relational aspects of working with other learners [6–10]. Research in nursing education examined the concept of personal comfort in simulation for elements that contributed to increased satisfaction and self-confidence within the simulation activity and found active learning to be the highest associated element [11]. However, it has yet to be examined how differences in solo or in group participation impact learner outcomes rooted in comfort and psychological safety.
This study aims to determine the perceived level of comfort during simulation training in those who have previously experienced group and solo scenarios compared to those who have previously experienced only group scenarios. Additionally, both were compared for differences regarding personal preference, perceived psychological safety, self-confidence, conduciveness to learning, realism and level of anxiety between the two simulation formats. In this regard, the perception of comfort when learning in a group or solo approach was viewed in how participants perceived learning outcome achievement. This study may guide future research to further uncover differences between these frameworks.
Furthermore, we seek to include the experience of varying disciplines, given the importance of identifying modalities applicable to a range of interdisciplinary bedside care professionals. We aim to uncover ways in which intentionality about the number of participants can support and maintain a focus on psychological safety by way of a learner-centred approach that is rooted in scenario design choices.
This is a cross-sectional, observational survey study of participants in healthcare simulation education at Carolinas Simulation Center (CSC) located in Charlotte, North Carolina. CSC is accredited by the Society for Simulation in Healthcare in Assessment, Research, Teaching/Education and Systems Integration and as a Comprehensive Education Institute by the American College of Surgeons. Participants were eligible for inclusion in the study if they were qualified healthcare professionals in their discipline and had previously participated in simulation prior to their currently scheduled activity. Participants were chosen based on their healthcare focus (nursing and physicians) after completing the required courses and examinations to begin working in their scope of practice. Therefore, physicians included were resident physicians who had completed medical school and were credentialed to work clinically in their practice area. Nurses included were those who had completed nursing school as well as certifications necessary to begin working clinically. Both the physician and nursing participants included in this study are new graduates and in their early career phase. Specifically, resident physicians are graduates of medical school but considered as medical trainees with licence to practise medicine while training. Physician participation included residents from the Departments of Internal Medicine, Pediatrics, Emergency Medicine, Psychiatry, Surgery, Urology, Orthopedics, Family Medicine, Obstetrics and Gynecology, and Physical Medicine and Rehabilitation. Nursing participants included Transition to Practice Program nurses employed in Intensive Care Units and Emergency Departments.
Those excluded were attending physicians, nursing educators, simulation centre staff, embedded participants and actors. Participants who attended the centre for procedural sessions or summative assessments were also excluded from completing the survey at that visit. Participants were invited to complete the survey at the start of their regularly scheduled simulation sessions while physically present at the simulation centre. Subjects were asked to complete the survey at the beginning of their learning activities for the day, and therefore prior to engaging in any new simulation activity. Prior to completing the survey, all participants viewed a short introductory video describing the study. The survey gathered information about the participants’ training background, previous healthcare simulation experience and comfort level with simulation training. Medical residents completed this survey as part of their introductory sessions at CSC at the start of their residency training. Nurses participated in this survey during their sessions at CSC as part of their Transition to Practice programme. Assuming a goal effect size of 1.5, the desired minimum sample size of each group (multiple learner and those who experienced both modalities) was determined to be 30 participants.
Nurses and medical residents were invited to complete a survey (Figure 1) during their previously scheduled educational activities at CSC in Charlotte, North Carolina, between June 2023 and November 2023. This survey focused on a retrospective recollection of personal sentiment regarding comfort, ability to engage and satisfaction in a wide variety of possible simulation environments experienced in prior learning instances. The survey contained de-identified responses regarding demographics, Likert-style questions (seven for each learning configuration) and optional free-text responses (two for each learning configuration). The Likert questions were initially modeled after question styles utilized in prior healthcare simulation research [6–8,11] as well as established guidelines concerning new survey formulation and testing [12–13]. Learners reported how much they experienced seven aspects of comfort, realism and satisfaction on a five-point Likert-type scale ranging from ‘not at all’ to ‘extremely’. We selected five-point responses because they have been shown to be more reliable than response scales with fewer items. Additionally, an odd-numbered scale allows for opportunity to capture the midpoint for respondents who may not have a definitive opinion. This may allow for future exploration, likely in the form of qualitative study, to explore fields in which participants lean towards a midpoint answer rather than a more definitive answer. The free-text responses were deemed optional and existed to obtain thoughtful and meaningful narrative responses.

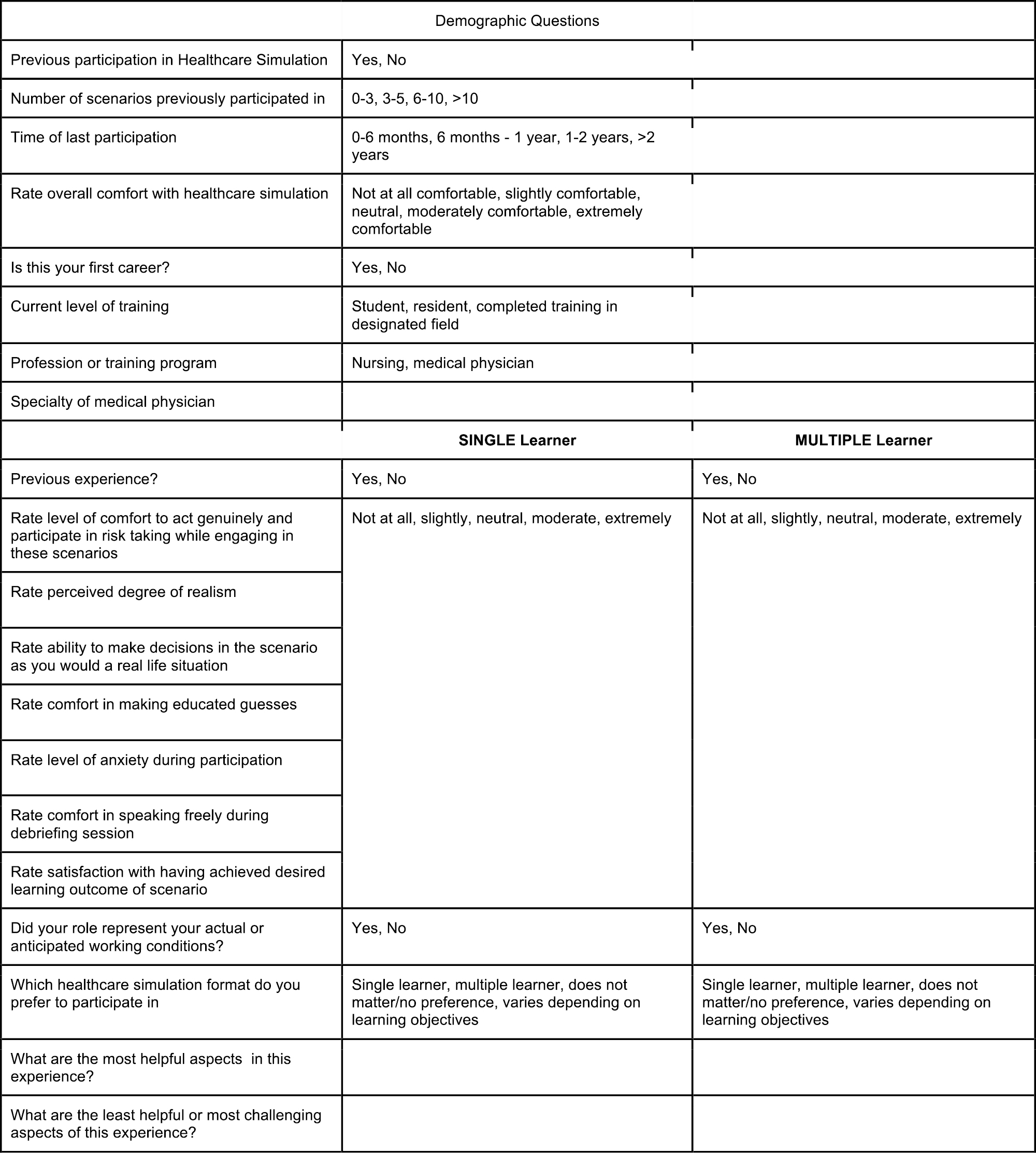
Healthcare simulation survey on previous experiences
No existing survey was found in literature review that measured our specific constructs of interest in the context of a healthcare simulation environment for multiple healthcare professions [16–19]. We therefore generated seven items to assess learners’ subjective experience of comfort and satisfaction with simulation-based learning experiences. Once our questions were created, then they were brought to a panel that reviewed the questions and provided feedback. The panel consisted of five experts (two physician simulation faculty content experts, one scientific writer with Certified Professional in Healthcare Quality certification, the director of clinical research within our department, the chair of our department’s Scholarly Oversight Committee) and four target population judges (learners in healthcare simulation who train at the same simulation centre as the participants who are also cleared for clinical practice and novice in status). Prior to finalization, the survey was additionally reviewed by two simulation nurse education managers with Certified Healthcare Simulation Educator certification. Questions were modified based on feedback from the panel and then brought back to the panel in an iterative manner for review following revisions. The panel reviewed the revised survey questionnaire again to create the final iteration of the scale.
Surveys were distributed through QR codes to participants prior to the start of their simulation sessions. The QR codes provided access to the secure survey on REDCap. This project was reviewed and judged to be exempt by the Wake Forest Institutional Review Board. Surveys were anonymous and had no bearing on the course work of the subjects. Faculty involved in the participants’ summative evaluations were not involved in study design, the implementation, nor able to access data collected.
Participants with both single- and multiple-learner experiences were compared to those with only multiple learner experiences. Descriptive statistics and chi-squared (p-value < 0.05) were used to describe the differences in demographics and training experiences between the two groups. The Goodman and Kruskal’s gamma was used to determine the association, if any, of the two study groups and each of the survey questions. Gamma coefficients of 0.01–0.09 demonstrate a weak association, 0.1–0.29 a moderate association and 0.3–0.99 a strong association. Measures of association were employed to determine the association, if any, with participants’ training experiences and their perceived comfort with healthcare simulation. Specifically, gamma was used to measure the strength of association with perceived comfort and age, perceived comfort and last simulation experience and perceived comfort and number of previous simulation experiences. Subgroup analyses were completed to ensure that the results were not skewed by outliers in the data set. The subgroup analysis examined participants with fewer than 11 previous healthcare simulations, participant age and time elapsed since the last simulation experience. Descriptive statistics and Goodman and Kruskal’s gamma were used in the subgroup analyses and compared to the overall results.
Although formal thematic analysis of free-text responses was outside the scope of the present project, two authors independently reviewed all free-text responses and anecdotally noted recurring themes in respondents’ comments in order to enhance our interpretation of quantitative results.
A total of 174 learners completed this survey, including 129 who responded to the optional open-ended questions about the strengths and challenges of both single- and multi-learner experiences. Only three learners had participated in single-participant simulation only and were not included in the analyses, resulting in an analytic sample of 100 nurses and 71 medical residents. Participants who completed both modalities (single and multiple participant, n = 84) were compared to those who only completed one modality (multiple participants, n = 87) (Table 1). The predominant modality of healthcare simulation in nursing education was multiple learner only (70%), whereas the majority of medical residents utilized both modalities (76%). There were 161 participants who completed at least three simulation scenarios in their educational careers (94.1%). There were 152 participants who completed their last simulation session within one year prior to completing this survey (88.9%).

| Multiple learner only, n = 87 | Single and multiple learner, n = 84 | |
|---|---|---|
| Age | ||
| 20–25 | 37 | 22 |
| 26–30 | 28 | 56 |
| 31–35 | 17 | 3 |
| 36–40 | 2 | 3 |
| >40 | 3 | 0 |
| Role in medicine | ||
| Nursing | 70 | 30 |
| Physician | 17 | 54 |
| Number of scenarios completed | ||
| 0–2 | 9 | 1 |
| 3–5 | 47 | 18 |
| 6–10 | 20 | 23 |
| >10 | 11 | 42 |
| Time since the last participation | ||
| <6 months | 36 | 51 |
| 6 months to 1 year | 40 | 25 |
| 1–2 years | 7 | 7 |
| >2 years | 4 | 1 |
To understand participants’ sentiment regarding their prior healthcare simulation experiences, we utilized Goodman and Kruskal’s gamma to determine the strength of association on the Likert scale responses. Table 2 demonstrates the strength of association of the outcomes with those who experienced both modalities as compared to those who experienced multiple participant scenarios only. Participants who experienced both modalities felt higher comfort levels, increased satisfaction with scenario outcome, increased ability to act genuinely and take risks (strong association > 0.3). They felt a moderate increase in ability to make educated guesses, speak freely, realism, ability to make decisions and decreased levels of anxiety (gamma 0.1–0.29).

| Outcome | Gamma | Strength of association |
|---|---|---|
| Overall level of comfort | 0.367 | Strong |
| Ability to make educated guesses | 0.298 | Moderate |
| Satisfaction with scenario outcome | 0.316 | Strong |
| Act genuinely and take risks | 0.426 | Strong |
| Speak freely | 0.223 | Moderate |
| Anxiety | −0.188 | Moderate association showing decreased anxiety with both types |
| Ability to make decisions | 0.216 | Moderate |
| Realism | 0.212 | Moderate |
The primary objective was to evaluate the perception of comfort in comparing those who had only participated in multiple learner simulation as compared to those who have experienced both modalities. To further investigate participants’ perception of comfort, subgroup analyses were performed to determine if other factors contributed to a strong association of comfort after experiencing both modalities (Figure 2). We found an even stronger association on overall comfort when comparing those with increased simulation experience (gamma = 0.492). Increasing age and decreased time since the last simulation participation showed a moderate association when evaluating the overall level of comfort.

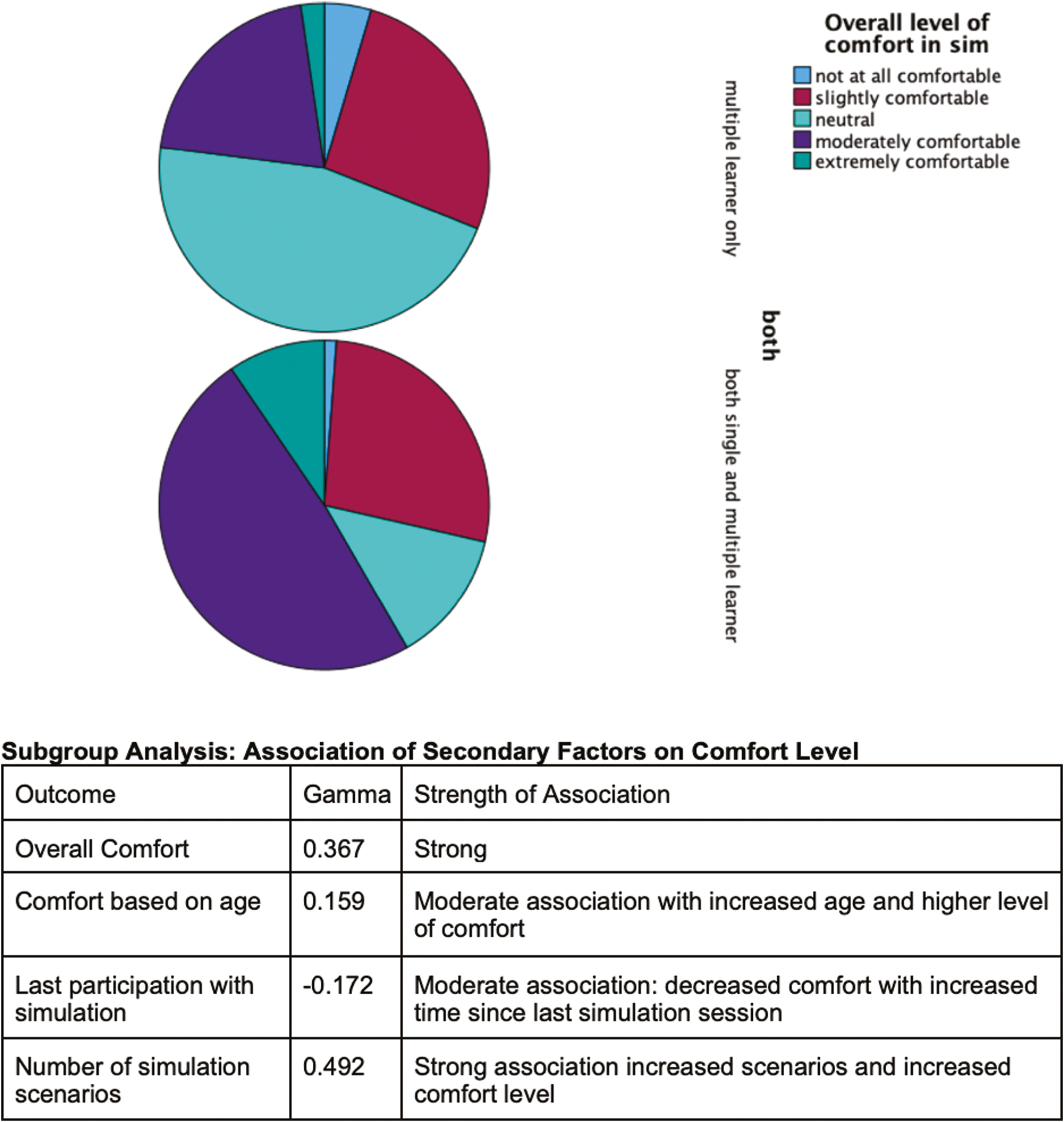
Analysis of comfort level of participants in healthcare simulation
A subgroup analysis was conducted for participants with less than 11 total simulation experiences prior to participation in this study to elucidate the strength of association with fewer total experiences. The level of association with both modalities was the same as the overall group for increased ability to make educated guesses, increased perception of realism, increased ability to make decisions, increased ability to act genuinely and take risks and decreased levels of anxiety. There was a higher association with increased comfort to speak freely (moderate to strong) and less of an association with increased satisfaction with scenario outcome and higher overall comfort (strong to moderate) in this subgroup.
All 129 free-text comments regarding the two modalities of healthcare simulation were reviewed informally; consistent recurring themes were identified by both reviewers and are highlighted in Table 3. Participants expressed that single-learner scenarios offered limited distractions and increased independence, autonomy and confidence. Additionally highlighted was being provided the opportunity to receive individualized and/or personal feedback in what was considered a more realistic approximation of real-world working conditions. Conversely, challenges participants experienced concerning single-learner scenarios were increased anxiety, pressure and lack of interprofessional collaboration (which was viewed as an important aspect of their day-to-day work responsibilities). Multiple learner scenarios emphasized communication, collaboration/learning from peers, realism and development of trust. Challenging aspects of multiple participant simulation included dealing with differing opinions which could result in confusion in the room, diffusion of responsibility (and thus unequal participation), less personalized feedback and difficulty in voicing opinions.

| Moderate | Ability to make educated guesses Speak freely Ability to make decisions Realism |
| Strong | Overall level of comfort Satisfaction with scenario outcome Ability to act genuinely and take risks |
Notes: A stronger association in these outcomes was demonstrated after experiencing both simulation modalities as compared to only experiencing multiple participant healthcare simulations. Feelings of anxiety were shown to have a decreased strength of association, meaning a decreased level of anxiety experienced by those who had only experienced multiple participant simulation
Simulation-based education (SBE) has emerged as one of the leading modalities to educate learners in various healthcare roles. In this study, we have taken an in-depth look at perceptions of comfort and psychological safety in single- and multiple-participant formats. We have seen which formats have high associations with factors that promote psychological safety and have then considered implications for design choices. Additionally, we have considered how the number of participants per scenario has implications that facilitators can carry through to the debriefing phase. We address each of these areas in the following sections in this discussion. We start with a section on leveraging participant number as an intentional design component, and the benefits of including a combination of solo and group modalities. We next discuss how collaborative learning can occur between participants to offset anxiety and increase the practice of teamwork-based skillsets. We then discuss the implications of how increased learner comfort promotes building and sustaining factors for psychological safety. Lastly, we review implications for learning within SBE, and how our findings can be used to promote a learner-centred experience to cultivate professional growth.
Our study demonstrates strong associations in comfort during performance, satisfaction with scenario outcomes and factors relative to psychological safety for those who experienced both solo and group learner scenarios. This would suggest the combined benefit of having participated in each framework optimizes the strengths that either format may offer individually. In the construction of a simulation curriculum, including opportunities to engage in both solo and group scenarios could be purposefully leveraged within a curriculum to maximize the exposure of both types. We theorize there may be a dynamic learning structure when the two overlap (Table 3), allowing for the challenges of one framework to be mitigated by working in the other framework for a synergistic effect. For example, the independence and confidence gleaned in working through a solo learner scenario may aid in the challenge of speaking up in a group. The lack of a collaborative team environment faced by solo learner scenarios may be contrasted against the interpersonal communication and role assignment practised within group scenarios.
The ability to target specific interventions in a longitudinal curriculum may be informed by these results. The strengths and weaknesses in single versus multiple learner experiences (Table 4) may be useful in identifying existing gaps or barriers to achieving desired learner outcomes within a given simulation curriculum. Additionally, given the strong association to act genuinely and take risks for those who participated in both frameworks, it may be prudent to lean towards a curriculum that incorporates the two with regular cadence. In this way, psychological safety is utilized to maximize learner impact towards the achievement of scenario outcomes.

| Helpful aspects | Challenging or least helpful aspects | |
|---|---|---|
Single learner |
• Independence • Confidence • One on one learning • Limited distractions • Autonomy • Self-sufficiency • Realism • Individual feedback |
• Anxiety • Pressure • Healthcare is a team environment/lack of realism • No interprofessional communication • Lack of collaboration |
Multiple learner |
• Communication • Teamwork • Collaboration • Realistic to work environment • Trust • Division of roles and responsibilities • Peer learning opportunities |
• Difficult to ‘speak up’ • Single person taking control • Clashing opinions • Overstepping or not fulfilling roles • Less personalized feedback • Easy to fade to background |
Note: Bold text indicates highest frequency of responses.
How learners learn from one another may be an underutilized tool within the simulationist’s toolkit. A theoretical framework known as situativity theory argues that knowledge, thinking and learning are rooted in one’s experiences and environment [14]. Durning et al. highlighted contributions of situativity theory in medical education attending to how participants interacting with one another can meaningfully impact learning [14]. We suggest the learner–learner relationship carries a potent ability to affect outcomes through titration of group participation in a curriculum and is rooted in the needs of the course. Participation as a solo learner includes the ability to reach core skills such as practising autonomy and self-efficiency. In healthcare training, these features may not have been otherwise achieved prior to entering clinical practice. Group-based scenarios offer robust grounds to engage in teamwork and collaboration, which can offset the missing team environment and heightened anxiety found in solo participant formats. In our study, this was consistent in resident physicians from multiple disciplines as well as nurses undergoing simulation-based training, suggesting a wide-based application of these concepts across healthcare professionals. In this regard, the educator may wish to maximize the creation of opportunities in which learners may learn from one another when implementing a group simulation scenario. This may be addressed through intentional design elements within a given scenario that encourage collaboration and problem solving during the case. Furthermore, these moments highlight debriefing topics that can be intentionally chosen to spotlight and reflect on. Collective debriefing on these moments of learner–learner collaboration provides the added benefit of having participants co-create solutions for clinical practice.
This initial study analyses individual sentiment regarding experiences in previous simulation scenarios. There was a strong association between increased overall level of comfort, satisfaction with the scenario outcome and ability to act genuinely and take risks when both formats were combined. We found a moderate increase in ability to make educated guesses and decisions, comfort to speak freely, perceived realism and decreased levels of anxiety after experiencing both single- and multiple-participant formats. These factors either directly or indirectly contribute to one’s psychological safety, a fundamental cornerstone of healthcare simulation. Optimizing aspects of psychological safety through healthcare simulation may translate to improvements in interprofessional interactions as well as bedside patient care [11]. Given the wide array of uses in healthcare simulations, scenario designers may encounter learners with highly variable backgrounds. In this regard, each learner arrives with varying degrees of past simulation experiences. Prior simulation experiences can be potent triggers for individual learners, as can the content for any given scenario. Trained facilitators are well versed in making deliberate choices to establish and maintain psychological safety during simulation-based learning experiences. We propose this may offer one aspect to implement a proportion of control towards building psychological safety, similar to how prebriefing is purposefully crafted towards building psychologically safe spaces. This may prove useful in the simulation space where there inherently lies a multitude of contributing factors that are otherwise out of the facilitator’s control. Importantly, we also demonstrated a strong association with satisfaction of scenario outcome. This provides foundations to build areas of future research that may target achievement of scenario objectives, ability to translate to bedside care or the impact to patient safety.
The number of participants per scenario may be determined by the preference of the designer, driven by logistical considerations or perhaps noncontributory to the initial design. Needs assessments obtained in the planning phases are often a well-defined pre-simulation step, yet it is less well described how scenario participation preferences fit into the design build. Prior study suggested there is no difference in one’s ability to obtain learning objectives in medical simulation when performed in a solo learner or group format [15]. While the number of participants per scenario has not previously been identified as contributory for or inhibitory against psychological safety of the learning environment, it may have implications in scenario design. The associations found through this study suggest that the choice of solo or group participation may serve to enhance learner comfort as it relates to feeling psychologically safe to participate. These features may be of interest to the simulation designer, the learners and the organization towards closing gaps and improving interpersonal interactions through SBE. Deliberate attention towards the features identified in the results of this study provides insight into which aspects may be relevant to a particular group of learners, offering an additional edge to reach a learner-centred approach. Furthermore, knowledge of learner perceptions for solo and group formats may inform debriefing conversations in placing intentional weight on topics which may be of greater or lesser interest within a particular organization or curriculum (Table 3). A debriefer could leverage this knowledge towards bolstering desired features or examining areas of struggle to uncover opportunities for participant-directed growth. The workflow of embedding psychological safety on the front end of the simulation design affords the ability to carry it through to the debriefing session. Prior work has been done on ‘explicit and implicit strategies to establish and improve psychological safety during debriefing’ as well as in ‘practices that have the potential to increase the likelihood of establishing and maintaining psychological safety in medical simulation’ [1, 20–22]. We propose the variability and intentionality of participant design choice may prove useful towards reaching organizational and curricular needs in SBE. We propose the next steps to further this work may be to explore the perceptions of learners within other organizations as it relates to single- and multiple-participant format, given organization culture variances may have differing effects.
Few respondents in the present sample experienced single-participant-only simulation (n = 3), and therefore the solo participant experience group was unable to stand on its own for consideration or analysis. This could be due to increased educational costs and resources required to perform individual simulation scenarios. Our participants came from various nursing schools and medical schools across the country, speaking to a significant variety regarding prior simulation experiences. Additionally, this survey did not include questioning about the manner in which these simulations occurred. Observed Structured Clinical Examinations are often utilized in the assessment of healthcare learners, and these often occur in a single-participant structure. This could skew results in those who had experienced both single- and multiple-participant simulation in the past if all single-learner experiences occurred during an assessment or examination. As this is a retrospective observational study, there are inherent biases based on study design alone. There could be recall bias as participants were asked about their previous experiences in healthcare simulation. Although 88.9% of respondents reported participating in simulation in the past year, there could be inherent bias depending on their individual experiences. It was shown that an increased number of simulation experiences resulted in increased overall comfort with simulation. A subgroup analysis looking at those with <11 previous simulation experiences was conducted to guarantee that the results were not biased and skewed by the group with more robust simulation experiences. The results were similar to those of the entire group, reinforcing the findings of the study. Understandably, those who participated in fewer total experiences reported less overall comfort as compared to those with increased experiences. This stresses the importance of optimizing and increasing learners’ engagement in healthcare simulation. Another limitation of this study is the lack of a formal thematic analysis of the 129 open-ended responses from participants. Although an informal review suggested valuable insights, a systematic qualitative analysis was not conducted. Therefore, it was outside the scope of this study to conduct focus groups or semi-structured interviews to explore participants’ feelings of comfort and psychological safety in detail. Importantly, this provides grounds for future research to formally analyse existing responses and gather additional qualitative data. This may provide a better understanding of the impact of group size and guide decisions about educational design.
This is the first study to evaluate the individuals’ perception of comfort and psychological safety regarding different participant structures in simulation scenarios among different disciplines within healthcare. Analysis of self-perceived learning preferences as well as emphasis on components of psychological safety will only further influence the development of curriculum in both nursing and medical education. Inclusion of both single- and multiple-participant simulation scenarios will provide a varied experience for learners that optimize psychological safety and carry implications for learner-centric outcomes. This approach begins with pre-design decisions and extends into debriefing practices to focus attention on components of interest. Further research should be conducted in broadening the ability to maximize benefit from both formats to build upon the impact of the relational learning structure within simulated healthcare scenarios. Additionally, comparing how different members of healthcare teams respond and engaging in a fully qualitative analysis on their experience surrounding psychological safety can provide increased insight into this topic.
The authors would like to acknowledge and thank Carolinas Simulation Center for their partnership and contributions.
AR1 is the primary author and developed the concept for the study. AR2 and MS provided support and development of methodology and study design. AR1, MS and AR2 undertook statistical analysis and data interpretation. LC is the senior author and provided support and oversight for concept. LC structured the manuscript and expanded upon writing the findings alongside AR1. All authors contributed to the review and editing of the final manuscript.
None declared.
This project was reviewed and judged to be exempt by the Wake Forest Institutional Review Board.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.