
In the interprofessional healthcare setting, foundation doctors are expected to to meet mental health competencies outlined in the UK Foundation Training Curriculum 2021 [1]. However, a lack of formal mental health education can lead to diminished confidence and skills in managing patients with acute mental health and physical clinical needs across various clinical settings (e.g. Emergency Department/ED, medical and surgical wards) in doctors and allied healthcare professionals. Recognizing this gap, a simulation-based programme was designed and piloted by foundation doctors, overseen by simulation faculty, to address the needs identified through analysis of cross specialty surveys amongst trainers and learners.
The aim of this study was to assess the effectiveness of a one-day learner-designed mental health simulation-based programme for interprofessionals in a tertiary London teaching hospital, featuring four common scenarios. The intended learning outcomes focused on management of acute mental health presentations, risk and safety assessment, application of relevant policies and legislation (e.g., CODE 10 policy, Mental Capacity Act/MCA, Mental Health Act/MHA), and de-escalation techniques. Simulated patient played by professional actors trained in mental health simulation were utilized in scenarios with support from facilitators and technicians, followed by debrief sessions after each scenario. Pre-course and post-course questionnaires, along with verbal feedback, were collected for evaluation.
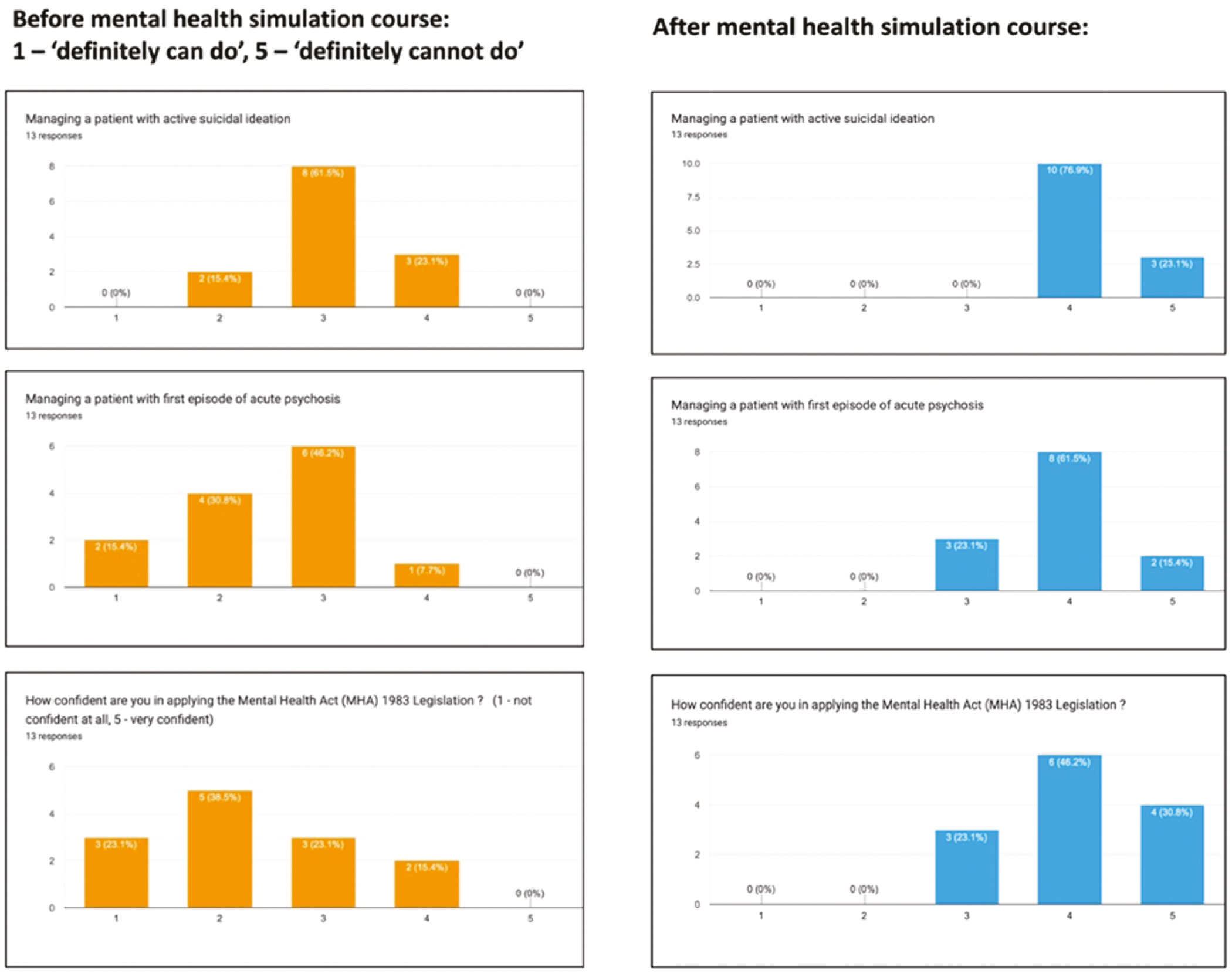
Thirteen professionals, comprising 7 doctors and 6 nurses including site nurse practitioner, participated in the programme. Before the course, only 8% of participants had formal mental health training. Only 62% of participants were aware that MHA Section 5(2) cannot be applied in ED. Analysis of pre- and post-course questionnaires revealed a significant increase in confidence levels across various scenarios, such as managing active suicidal ideation (77% uncertain vs. 100% somewhat confident), acute psychosis (92% uncertain vs. 77% somewhat confident), delirium on background of schizophrenia, substance misuse (delirium tremens in acute alcohol withdrawal) and personality disorders (PD), such as borderline PD (BPD). Notably, there was enhanced understanding of CODE 10, de-escalation skills, and application of MHA legislation post-simulation (Figure 1-A33). Participants unanimously found the programme highly useful, citing that high fidelity level was maintained in scenarios with acquisition of soft skills including multi-disciplinary teamwork and prioritization of self-care, psychological and physical safety.

This study underscores the effectiveness of an interprofessional mental health simulation-based programme designed by learners in bridging the gap in formal mental health education and delivering compassionate, timely and safe mental health care to meet the emerging demand across the NHS.
Authors confirm that all relevant ethical standards for research conduct and dissemination have been met. The submitting author confirms that relevant ethical approval was granted, if applicable.
1. Health Education England. UK Foundation Programme Curriculum 2021 [Internet]. UK Foundation Programme NHS. 2021 [cited 2023 Oct 21]. Available from: http://foundationprogramme.nhs.uk/curriculum.
Thank you to simulation faculty, development and technical team, staff from medical and surgical teams, nursing team, senior site nurse manager team, liaison psychiatry team and emergency medicine team who gave invaluable advice on all aspects of the pilot study including scenario design, teaching materials and with running of the pilot simulation programme.