
Most foundation doctors within the UK provide patient care out-of-hours, working with greater independence and a more intense workload than during in-hours. Despite this, there is a lack of on-call experience for medical students, with new Foundation Year 1 (FY1) doctors reporting significant anxiety, particularly when forced to work beyond their competencies [1]. Increased anxiety is linked to higher rates of medical errors [1]. Concerning rises in death rates during junior doctor changeover in August has further compounded these worries, prompting action to resolve this issue [2]. We created a simulated out-of-hours on-call shift to better prepare final-year medical students for the transition to FY1.
Eight simulated ward-based tasks were created involving data interpretation, documentation and prescribing. These simulated patient materials were placed in clinical environments around the hospital. The session began with students being handed over a job from the day team, with regular bleeps to direct them to further stations. The session concluded with a simulated cardiac arrest and a discussion on resuscitation. Senior doctors were available through a simulated switchboard, which students could call anytime. The following day, a debrief took place with accompanying teaching and feedback on overall student performance. Students were asked to complete a pre- and post-session questionnaire to provide feedback and guide the future development of the simulation.
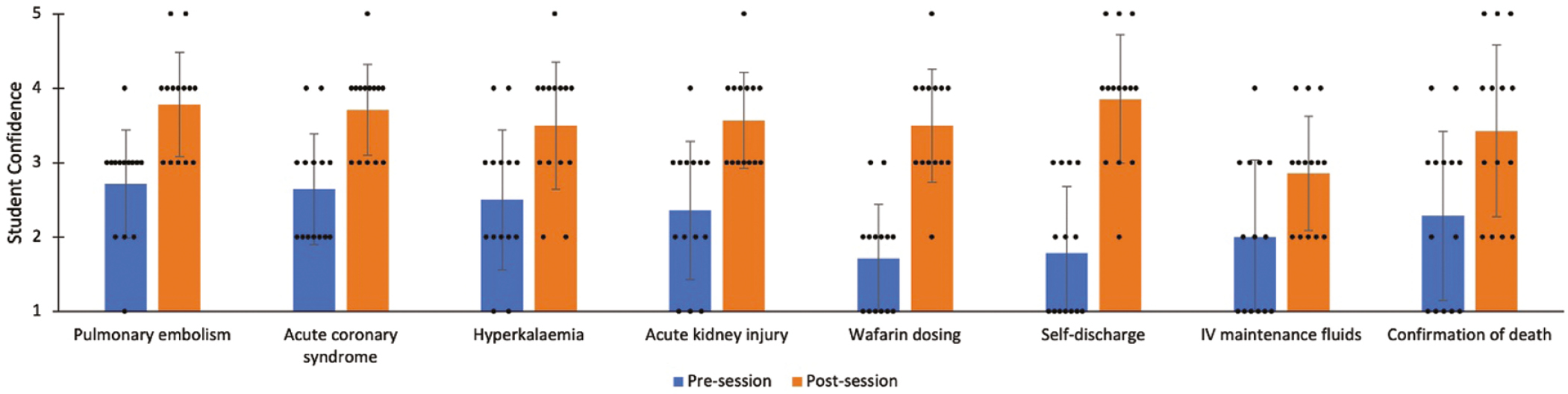
Fourteen final-year medical students from two universities completed the same simulation over two evenings. Students reported a mean increase in self-rated confidence across all eight scenarios (Figure 1-A46). Students also reported self-rated improvements across seven skills domains, including working within their competencies, high-risk prescribing and knowing when to escalate to seniors using a structured handover. Only four students had prior on-call experience, but all 14 reported that the session increased their insight into what is expected of an FY1 on-call.

Although participant numbers were small, students reported significant improvements in their readiness to start FY1. This highlights the importance of on-call experiences in the medical education curriculum to ease the transition from student to doctor. Arranging equivocal experiences shadowing junior doctors is challenging; however, simulation offers a safe space to mimic independent patient care, an infrequent experience for medical students. The nuances of patient care at our site may differ from that of the students’ first FY1 rotation, e.g. electronic vs paper prescribing. This may limit the simulation’s impact however further work in the area can help to maximise its benefits.
Authors confirm that all relevant ethical standards for research conduct and dissemination have been met. The submitting author confirms that relevant ethical approval was granted, if applicable.
1. McCullough JH, van Hamel C. Anxiety among newly-qualified doctors: An eight-year analysis. Medical Teacher. 2019;42(1):52–57.
2. Jen MH, Bottle A, Majeed A, Bell D, Aylin P. Early in-hospital mortality following trainee doctors’ first day at work. PLoS ONE. 2009;4(9).